As flu season arrives in the U.S., researchers worry that adults preoccupied with the COVID pandemic might forget or forgo a flu shot this year.
They’re concerned about low immunization rates, particularly among some racial and ethnic minorities, because unvaccinated adults are more likely to develop severe illness and need hospitalization. Health experts also worry about a “twindemic” resulting from the ongoing COVID-19 pandemic and flu season.
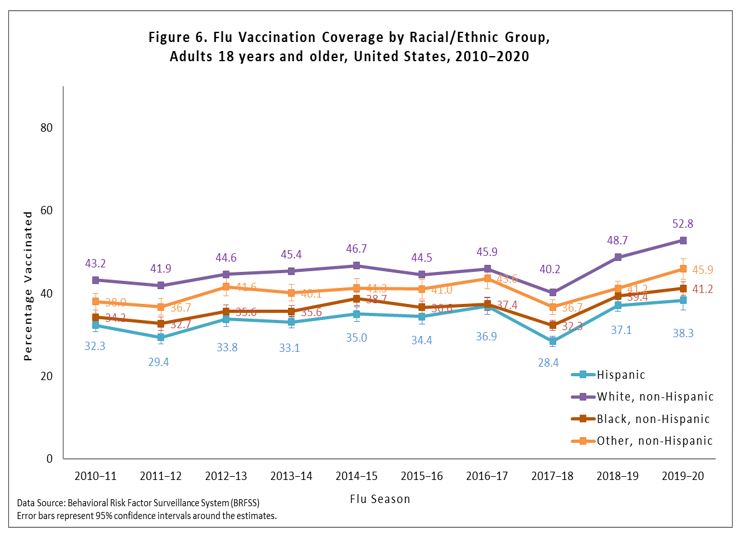
Healthy People 2030, the federal government’s prevention agenda to build a healthier nation, has set a goal of inoculating 70% of the U.S. population against the flu each year. Yet, the most recent data, from the 2017-18 flu season, show that 46.1% of U.S. adults aged 19 years and older had received the flu vaccine during the influenza season. Coverage rates were lower among Black (39%) and Hispanic (37.5%) adults.
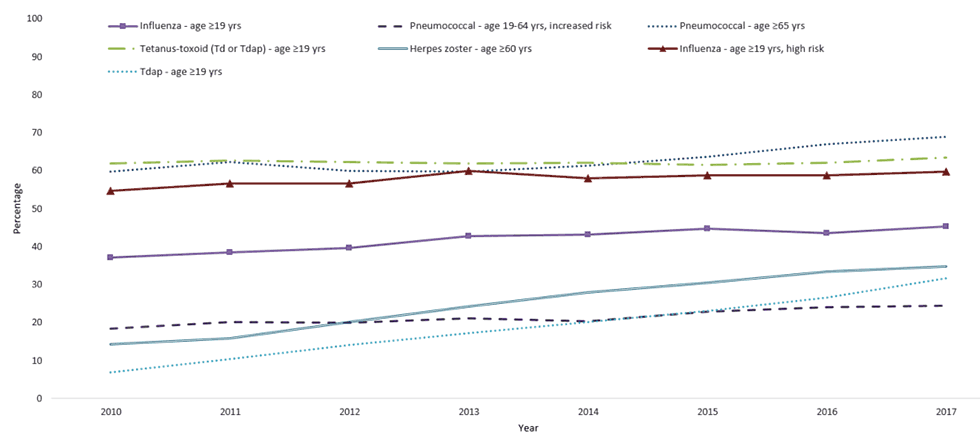
The scope of shortfalls in adult vaccines goes beyond flu shots. Each year, the Centers for Disease Control and Prevention updates its vaccine recommendations in the U.S. Adult Immunization Schedule, taking into account several factors including age, prior vaccinations and underlying health conditions. In addition to influenza, the vaccines include pneumococcal disease, herpes zoster (shingles), and Tdap (tetanus, diphtheria and pertussis).
But studies that have analyzed immunization trends for the recommended vaccines consistently show that many adults don’t get their recommended shots. Immunization rates among Black and Hispanic adults in the U.S. have been persistently lower for all recommended vaccines compared with white and Asian populations.
Meanwhile, Black adults have the highest flu-related hospitalization rate in the U.S. — nearly twice as high as white individuals, according to the U.S. Centers for Disease Control and Prevention.
“Three out of four adults are not caught up with their vaccinations and that is going to result in morbidity, mortality and [health care] costs,” says Litjen “L.J” Tan, chief policy and partnership officer at the nonprofit Immunization Action Coalition, who helped draft and publish “A Call to Action to Protect All Adults from Vaccine-Preventable Disease and Disability,” in August, urging health care providers to take action to improve routine vaccination of adults. The National Adult and Influenza Immunization Summit’s call to action was highlighted and endorsed by the CDC.
The call to action was partly driven by the pandemic, but also by the chronically low adult vaccination rates overall, says Tan, who is also co-chair of the National Adult and Influenza Immunization Summit.
“If we had done our [adult] vaccinations well before COVID, we wouldn’t have had the struggle that we have now,” he says.
Educating adults about vaccines and why they’re safe and effective could have helped reduce the vaccine hesitancy that we face today, he adds.
There are several reasons for low adult vaccination rates and persisting disparities.
For one, routine physician check-ups wane as children enter adulthood and “provider recommendation is extremely important for an adult to get vaccinated,” says Tan. Another barrier is access to vaccines, he adds.
Other factors include lower level of education and income, racism, lack of access to health care and transportation, and a lack of trust in the health care system due to experiencing racism in the past.
Tan hopes the systems that are being put into place now to vaccinate adults against COVID-19 will help improve coverage for other adult vaccines.
“Don’t let it just go away because the crisis goes away,” Tan says.
Below, we’ve gathered several studies that further parse out disparities in adult immunizations.
Research roundup
Racial/Ethnic and Socioeconomic Disparities in Adult Vaccination Coverage
Kosuke Kawai and Alison Tse Kawai. American Journal of Preventive Medicine, October 2021.
The study analyzes trends in influenza, pneumococcal disease, herpes zoster (shingles), and Tdap (tetanus, diphtheria and pertussis) vaccination coverage using the National Health Interview Surveys from 2010 to 2019, including a total of 311,343 adults. It shows even though overall adult vaccination rates increased between 2010 and 2019, many gaps remain.
Conducted annually in person among a nationally representative sample of adults, the National Health Interview Survey collects data on demographics, health status, insurance coverage and access to health care. It is one of the major data collection programs of the CDC’s National Center for Health Statistics. The survey collects self-reported flu and Tdap vaccination information from adults aged between 18 and 64 years. For those aged 65 and older, it collects self-reported flu, Tdap, pneumococcal and shingles vaccination information.
The study reveals several trends. Overall, white adults are more likely to receive their recommended shots than Black and Hispanic adults. Also, older adults (65 years and up) have higher vaccine coverage than those under 65. Low household incomes and low education levels were associated with lower vaccine uptake. Also, adults without health insurance had a substantially lower uptake of vaccination compared with those who had health insurance, the study shows.
“Promoting health equity in immunization rates for the new vaccines against COVID-19 during the pandemic is critical because individuals from racial and ethnic minority groups are disproportionately affected by COVID-19,” the authors write. “Efforts are urgently needed to achieve equity in immunization rates.”
Socioeconomic disparities in vaccination coverage rates have persisted among adults aged 65 years and older, the study shows. The authors say some of the barriers for this age group include concerns about out-of-pocket costs and low stock in doctors’ offices due to the cost of storing the vaccines.
To improve adult vaccination rates, researchers offer several solutions.
Reminders from providers and standing orders from health care providers have been found effective in reducing disparities, they write. Large-scale programs that distribute and administer vaccines to uninsured and underinsured adults could also be effective. Another effective model is the Vaccines for Children program, which is a federally-funded entitlement program that provides free vaccines to uninsured and underinsured children. The program has been credited with narrowing racial and ethnic disparities in children’s immunization rates in recent decades.
Surveillance of Vaccination Coverage Among Adult Populations — United States, 2018
Dr. Peng-Jun Lu; et al. Morbidity and Mortality Weekly Report, May 2021.
The study analyzes data from the 2017 and 2018 National Health Interview Survey, in which a total of 25,307 adults aged 19 years and older participated. It shows persisting racial and ethnic disparities in vaccination rates for several adult vaccines, including flu, pneumococcal disease, shingles and tetanus shots.
The study also shows that having health insurance coverage, having a usual place to receive health care and having one or more interactions with a doctor during the prior year are associated with higher vaccination rates.
“Awareness of the need for vaccines for adults is low among the general population, and adult patients rely on provider recommendations for vaccination,” the authors write. “Because of COVID-19-related reductions in persons accessing vaccination services, it is important to assess the vaccination status of all patients at each visit to avoid missed opportunities for vaccination and ensure timely vaccine catch-up.”
The study also looks at vaccination coverage among health care providers, showing that immunization rates among those with direct patient contact is higher than those without direct patient care. For instance, in 2018, 72.6% of health care providers with direct patient care got their flu shot compared with 70.5% of those without direct patient care. Among those with direct patient care, flu vaccine coverage among white providers (72.3%) was similar to coverage for Black providers (75.0%) and Hispanic providers (70.3%), the analysis shows.
Those numbers, however, fell below the Healthy People 2020 target of 90% coverage, according to the study.
Meanwhile, white providers with direct patient care had higher rates of hepatitis B vaccine coverage (82.3%) compared with Black providers (58.1%) and Hispanic providers (62.6%).
Vaccination Coverage Among Adults in the United States, National Health Interview Survey, 2017
Mei-Chuan Hung; et al. U.S. Centers for Disease Control and Prevention, February 2018.
The study summarizes data on vaccination coverage for U.S. adults aged 19 years and older using data from the 2016 and 2017 National Health Interview Survey of 33,028 and 26,742 adults, respectively. The vaccines included in the study are influenza, pneumococcal disease, shingles (herpes zoster) and tetanus (Td and Tdap).
Researchers find that only one quarter of adults aged 19 to 64 years who were at increased risk of invasive pneumococcal disease because of underlying health conditions reported ever receiving a dose of pneumococcal vaccine. In addition, 60% of adults at high risk of flu complications were vaccinated in the 2016-2017 influenza season, leaving 40% of high-risk adults unprotected.
Consistent with other studies, the analysis shows that even though overall vaccination rates increased between 2016 and 2017, white adults in the U.S. had higher rates of vaccination compared with people of color.
“Large disparities in vaccination coverage by race/ethnicity have remained mostly unchanged over the last several years, with white adults having the highest coverage for most vaccines and age groups,” the authors write. “Achieving significant improvements in overall coverage while reducing racial/ethnic disparities will require action at multiple levels of the healthcare system.”
Influenza Vaccination Coverage Among Adults by Nativity, Race/Ethnicity, Citizenship, and Language of the Interview United States, 2012–13 Through 2017–18 Influenza Seasons
Meagan Chuey; et al. American Journal of Infection Control, September 2021.
The study analyzes the differences in influenza vaccination rates during the 2012-2013 through 2017-2018 flu seasons using the National Health Interview Survey. It finds that while flu immunization rates improved among U.S.-born adults, they didn’t change significantly among foreign-born individuals, particularly among non-U.S. citizen adults.
The annual sample size ranged from 24,000 and 33,000, of which 17.7% to 18.9% were foreign born. More than half of foreign-born respondents were naturalized U.S. citizens. Also, most white and Black adults were born in the United States, while most Hispanic and Asian respondents were foreign born.
Foreign-born adults had significantly lower vaccination rates than U.S.-born adults for most flu seasons in the study. Their vaccination rate in the 2017-18 flu season was 4.5 percentage points lower (42.4% vs. 46.9%, respectively), the study shows.
The findings are important because foreign-born individuals represent 17% of the U.S. workforce and are more likely to be essential workers with jobs in the health care and food production industries, researchers write.
“Achieving high influenza vaccination coverage among the foreign-born population will help reduce illness among the essential workforce, achieve national vaccination goals, and reduce racial and ethnic disparities in vaccination coverage in the US,” they write.
The authors list several potential reasons for the disparity.
“Foreign-born populations experience inequities in socioeconomic conditions and access to health care and preventive services that are negatively associated with vaccination coverage,” they write. “Foreign-born adults may also be less aware of US adult immunization recommendations or have different attitudes toward vaccinations.”
Trends in Place of Early-Season Influenza Vaccination Among Adults, 2014-15 Through 2018-19 Influenza Seasons — The Importance of Medical and Nonmedical Settings for Vaccination
Peng-jun Lu; et al. American Journal of Infection Control, May 2021.
Analysis of data from the 2014 to 2018 National Health Interview Survey shows that increasing access to flu vaccines — whether it’s at the doctor’s office, workplace, supermarket or pharmacy — is important in improving immunization rates.
The doctor’s office was the most common place for receiving the flu vaccine, followed by the pharmacy and workplace, the study shows. But the study also shows racial and ethnic differences in where people get vaccinated. Black and Hispanic adults were significantly more likely to receive their flu vaccine in medical settings and less likely to receive it in nonmedical settings like the pharmacy and workplace compared with white adults.
“These associations may result from place of vaccination preferences, differences in vaccine-seeking behavior, differences in availability of nonmedical settings offering vaccinations, or disparate availability of workplace vaccination among socioeconomic groups,” the authors write.
Influenza-Related Hospitalizations and Poverty Levels — United States, 2010–2012
Dr. James Hadler; et al. Morbidity and Mortality Weekly Report, February 2016.
The study shows that flu hospitalization rates in neighborhoods where 20% or more of the residents lived below the federal poverty level were twice as high as in areas where less than 5% of people lived below the federal poverty level. In other words, people who lived in high poverty neighborhoods had a higher risk of severe flu outcomes.
Researchers say some of the contributing factors include lower vaccination rates among people who live in poorer neighborhoods, poverty-related crowding that can lead to more flu transmission and higher rates of underlying medical conditions that increase the risk of severe flu.
The study authors recommend increasing vaccination rates in poor neighborhoods and improving access to antiviral medications at clinics and doctors’ offices.
Primary Care Physicians’ Perspective on Financial Issues and Adult Immunization in the Era of the Affordable Care Act
Dr. Laura Hurley; et al. Vaccine, January 2017.
In an internet and mail survey of 317 general internists and 236 family physicians, 24% to 30% of the respondents said, “adult patients defer or refuse certain vaccines for financial reasons most of the time.” Also, 35% said they didn’t recommend vaccines because they thought the patient’s insurance wouldn’t cover it. Meanwhile, 37% were “not at all aware” of the vaccine coverage provisions of the Affordable Care Act.
“Physician recommendation is critical to patient receipt of vaccines, yet we found that physicians are not recommending vaccines to adults for financial reasons,” the authors write. “Regardless of actual insurance coverage, if physicians perceive that vaccines are not covered, they may not recommend them.”
Early-Season Influenza Vaccination Uptake and Intent Among Adults — United States, September 2020
Megan Lindley; et al. U.S. Centers for Disease Control and Prevention, December 2020.
In an online survey, a nationally representative sample of 3,594 U.S. adults were asked about their intent to get the flu shot for the 2020-21 influenza season. Results reveal the COVID-19 pandemic didn’t have a substantial effect on the general public’s attitude toward the flu vaccine. The proportion of people who said they intended to get the flu shot was slightly higher — 59% versus 52.2% in the 2019-2020 flu season — but demographic differences remained largely similar to previous flu seasons, according to the study.
“Particularly concerning are the disparities in vaccination intent by race/ethnicity: approximately half of Black and Hispanic respondents reported intent to receive influenza vaccination compared with 61% of White respondents and 65% of other-race respondents,” the authors write.
Additional information
The CDC has several vaccine reports, some of which are updated regularly:
- Recommended adult vaccine schedules.
- Flu vaccine coverage by season.
- Annual flu vaccination coverage estimates in the U.S.
- Weekly U.S. influenza surveillance report.
- COVID-19 vaccinations by race and ethnicity.
The Kaiser Family Foundation, a nonprofit health policy think tank, issued a report on Sept. 9 about COVID-19 vaccination by race and ethnicity.


Expert Commentary