This piece, originally published in July 2021, was updated in May 2024 with new data from the Centers for Disease Control and Prevention and the findings of two recent studies on drowning prevention interventions.
Worldwide, at least 235,000 people fatally drown each year, making it one of the leading causes of injury-related death. The U.N. General Assembly has said drowning is “largely unrecognized relative to its impact.”
In the United States, drowning deaths are on the rise after decades of decline. More than 4,500 people drowned each year from 2020 to 2022, according to the most recent data from the Centers for Disease Control and Prevention. That’s about 500 more drowning deaths each year compared with 2019, the agency reported.
While local news stories about drownings — fatal or non-fatal — often focus on single events, journalists have the power and responsibility to inform their audience with statistics, trends and research on prevention. As noted in a 2019 report in the Health Promotion Journal of Australia, “Transmission of messages about drowning risk factors and prevention strategies, during summer, may lead to behavior change at a time when drowning risk is highest.”
Drowning is medically defined as the process of experiencing respiratory impairment from submersion or immersion in liquid. Drowning can be fatal, non-fatal with no injuries or non-fatal with injuries. In the U.S. there are about twice as many non-fatal drownings each year, which can lead to long-term health problems and costly hospital stays, according to the CDC.
This explainer includes information on fatal drowning trends over the past two decades; the findings of three recent reports on racial disparities in fatal drowning rates; the factors contributing to disparities in drowning death rates among Black, Alaska Native and American Indian youth; the role of socioeconomic status; the role of climate change and the COVID-19 pandemic; and, finally, research on prevention.
An overview
Downing deaths differ by age and race and ethnicity.
For children aged 1 to 4, drowning rates increased by 28% in 2022 compared with 2019. For adults aged 65 to 74, drowning rates increased by 19% in that period, according to the CDC.
Among racial and ethnic groups, American Indian or Alaska Native people have historically had the highest rates of drowning deaths, followed by Black people. In 2021, drowning deaths among Black people increased by 28% compared with 2019, while the rates remained unchanged for AIAN people, the 2024 CDC data shows.
The greatest percentage of drowning deaths in babies under 1 year occur in bathtubs; in swimming pools in children between 1 and 13; and in natural bodies of water such as lakes, rivers, streams, and oceans in youth between ages 14 and 17, according “Unintentional Drowning Deaths Among Children Aged 0–17 Years: United States, 1999–2019,” released in July by CDC’s National Center for Health Statistics.
Some groups, including males, children and people with underlying medical conditions have a higher risk of fatal drowning. Also, factors like inability to swim, lack of close supervision, place of swimming and use of alcohol during water activities make drowning more likely.
In the U.S. roughly 40 million adults don’t know how to swim, including 37% of Black adults, compared to 15% of all adults. More than 60% of Black adults and 72% of Hispanic adults reported never taking a swimming lesson, the latest CDC data shows. Among all adults, nearly 55% have never taken a swimming lesson.
In the 2018 study “Predictors of Swimming Ability among Children and Adolescents in the United States,” published in Sports, researchers found that parents have a strong influence on kids’ ability to swim. Other factors that were positively associated with swimming ability included knowledge of water safety, having access to pools that were open all year and having a best friend who enjoys swimming.
There are still many unanswered questions about drowning, partly due to gaps in data and lack of research.
Many studies that look at fatal drowning data use death certificates, which don’t have information on the circumstances of drowning, details of known risks or other potential social or cultural influences, leaving a gap in better understanding of drowning data.
In addition, there are fewer studies on drowning compared with other unintentional injuries.
In “NIH Portfolio of Unintentional Injury Research Among Racial and Ethnic Minority Children: Current Landscape and Future Opportunities,” published in the Journal of Racial and Ethnic Health Disparities in July 2020, researchers found that between 2011 and 2018, 130 NIH-funded grants examined unintentional injuries — fatal and non-fatal — such as burns, drownings, falls, poisoning and car accidents. Of those, 34 were focused on children. And of the 34, eight focused on racial and ethnic minority children. Of the eight, half studied car injuries and none focused on drowning.
“In my mind, drowning prevention is the poor cousin in injury prevention,” says Dr. Linda Quan, a professor in the Department of Pediatrics at the University of Washington School of Medicine whose area of research includes drowning prevention and pediatric resuscitation. For motor vehicle injuries, which have received far more attention, there’s the National Highway Traffic Safety Board, or NHTSA, at the federal level. “But we don’t have really any kind of unity or single organization to push drowning prevention,” she says.
In “Interventions associated with drowning prevention in children and adolescents: systematic literature review,” published in Injury Prevention in 2015, researchers looked at academic literature about drowning prevention in children and teens, published between 1980 and 2010, and found that “few studies employ rigorous methods and high levels of evidence to assess the impact of interventions designed to reduce drowning.” The studies, the authors wrote, lacked consistency in measuring outcomes and the use of drowning terminology.
For instance, the study authors use the terms “fatal” and “non-fatal” drowning instead of “immersion,” “submersion,” “drowning” and “near drowning.”
“Terms such as ‘near-drowning,’ ‘dry or wet drowning,’ ‘active and passive drowning,’ ‘secondary,’ and ‘delayed onset of respiratory distress’ should not be used,” according to BMJ Best Practice.
Another term used by researchers is “water competency.” Water Safety USA, a roundtable of several national nonprofit and governmental organizations with a focus on drowning prevention and water safety programs, defines water competency as the ability to anticipate, avoid and survive common drowning situations in addition to being able to recognize and provide assistance to those in need. It also includes water safety awareness, basic swimming skills and helping others.
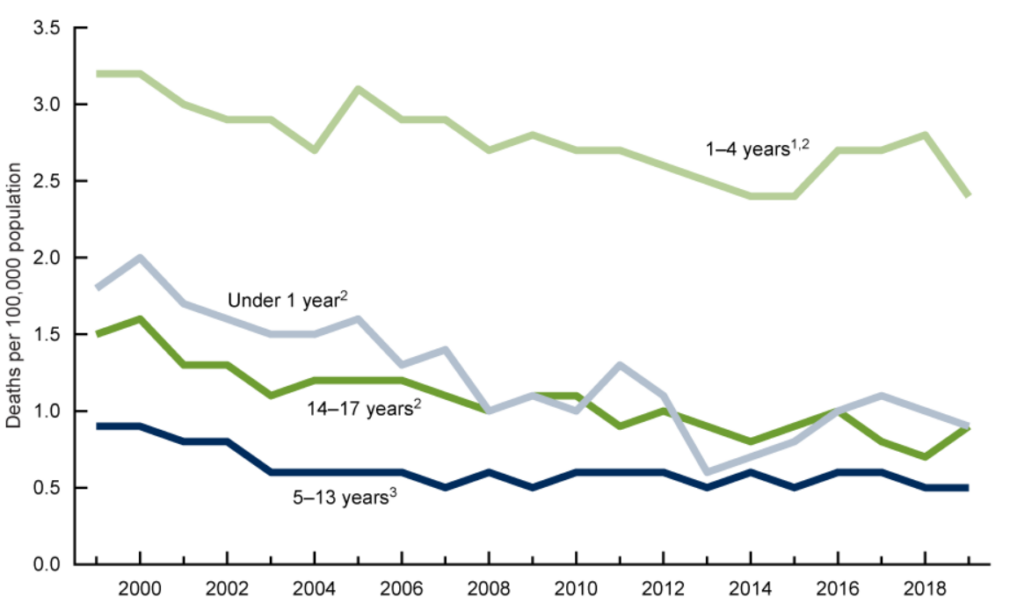
To be sure, drowning death rates declined by 32% in the U.S. and 57% worldwide between 1990 and 2017, thanks to educational campaigns and increased awareness. The rate of unintentional drowning deaths among children aged 0 to 17 years declined 38% in the U.S., according to the CDC report. But disparities in certain racial and ethnic groups have persisted.
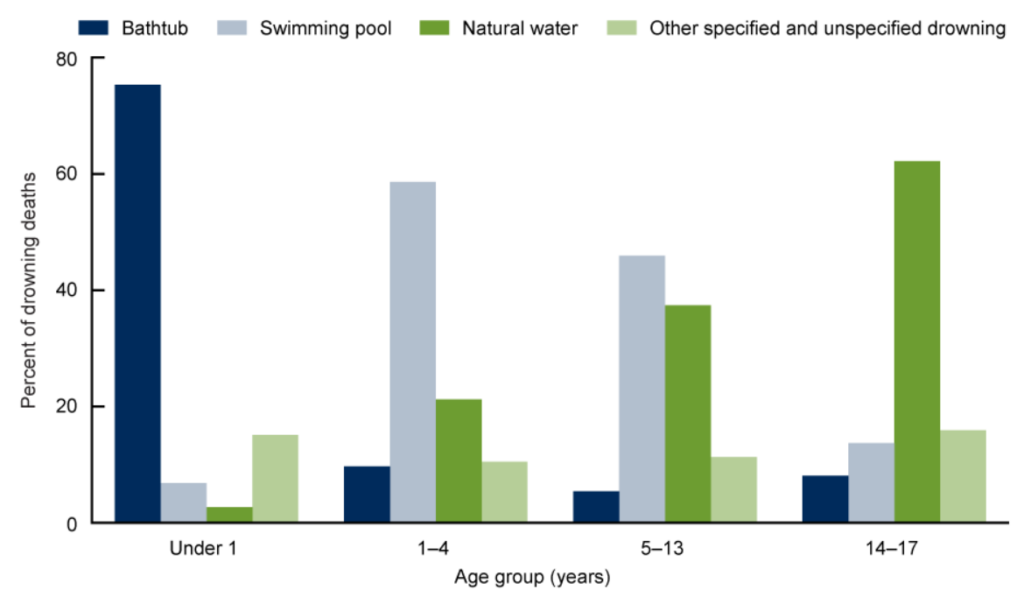
Source: National Center for Health Statistics’ study “Unintentional Drowning Deaths Among Children Aged 0–17 Years: United States, 1999–2019.”
Three 2021 reports to help you report on disparities in drowning deaths
Three reports released in June and July show that some racial disparities in drowning deaths exist and have persisted for more than 20 years, even though overall drowning death rates have declined.
Each report focuses on a slightly different age group, but they all show similar trends by age, sex, place of drowning, race and ethnicity.
Specifically, the reports show that disparities in drowning death rates are largest among Black, American Indian and Native Alaskan youth compared to whites, while there are little or no disparities among Hispanics, Asians, Pacific Islanders and whites.
The first study, “Persistent Racial/Ethnic Disparities in Fatal Unintentional Drowning Rates Among Persons Aged ≤29 Years — United States, 1999–2019,” published in the June 18 issue of CDC’s Morbidity and Mortality Weekly Report, shows that the drowning death rate among American Indian and Alaska Native people under 30 was twice as high as the drowning death rates for white people, while the rate for Black people was 1.5 times that of whites.
“Disproportionately high drowning death rates among certain racial and ethnic groups represent an important health equity issue,” says Dr. Tessa Clemens, a health scientist in the division of injury prevention at the CDC and one of the authors of the CDC study. “So, I think progress towards eliminating drowning in the United States, which is our goal — for there to be zero drowning — will only occur if we address these inequities and reduce drowning death rates in all groups.”
Fear of drowning has been identified as one factor contributing to limited swimming ability in some Black youths, write the authors. They point to the 2019 study “Vanishing Racial Disparities in Drowning in Florida,” published in Injury Prevention, which shows a reduction in drowning disparities between Black and white children potentially due to community-level initiatives to teach Black children how to swim.
The authors also point out an important limitation in the death certificate data, which they used for their study: the race and ethnicity on death certificates are reported by next of kin or by observation and people who identify as American Indian/Alaska Native, Asian or Hispanic are sometimes reported as white or non-Hispanic on death certificates, “leading to possible underestimations of deaths among these groups,” the authors write. “Proxy reporting of race/ethnicity is especially inaccurate for AI/AN persons.”
A 2016 CDC Vital and Health Statistics report “The Validity of Race and Hispanic-origin Reporting on Death Certificates in the United States: An Update,” found that while reporting for whites and Blacks has been “excellent” and had improved between 1979 to 2011 for Hispanics and Asian or Pacific Islanders, it has been poor for American Indian or Alaska Natives, where as many as 40% were misclassified on death certificates. The decedent’s country of birth and the racial and ethnic composition of where they lived at death have important effects on the quality of death certificate race and ethnicity reporting, the authors write.
“So an important message that we have in this study is that further research is really needed on the determinants that contribute to these disparities so that we can understand what’s driving them and what are the barriers to implementing effective drowning prevention programs in the communities that are at highest risk of drowning,” says Clemens.
United States, 1999–2019.
Source: National Center for Health Statistics’ study “Unintentional Drowning Deaths Among Children Aged 0–17 Years: United States, 1999–2019.”
The second report of note is the American Academy of Pediatrics’ technical report “Prevention of Drowning,” released in mid-July and forthcoming in the August issue of Pediatrics. It shows that from 2014 to 2018, in babies and children under 19, fatal drowning rates were highest among Black and American Indian and Alaska Native individuals. And while most white children died in residential pools, Black youths were most likely to die in a public pool, often at a motel or hotel.
Many times those pools are not supervised or don’t have a lifeguard on duty, says Quan, who is one of the study’s co-authors.
The American Academy of Pediatrics’ report also notes that there is “no data to support a recommendation for infant swim lessons. Aquatic programs for young children (especially those younger than 1 year) pose some medical concerns, and initiation of a swim program should be discussed between an infant’s caregiver and pediatrician.”
And the third report, “Unintentional Drowning Deaths Among Children Aged 0–17 Years: United States, 1999–2019,” released in July by CDC’s National Center for Health Statistics, shows that in the study’s two-decade period, fatal drowning rates were higher for Black children than for white or Hispanic children. Rates were also higher for children living in rural counties compared with urban counties. After declining from 1999 through 2003, the unintentional drowning death rate for Black children remained stable from 2003 through 2019, the report shows. Meanwhile, drowning rates for white and Hispanic children showed a steady decline during those years.
Drowning disparities among Black youth
Some of the contributing factors to higher drowning rates, particularly among Black children, are poor swimming skills in both children and their parents, lack of swim training during childhood, and lack of lifeguards at motel and hotel pools, according to the American Academy of Pediatrics’ new report.
“With no physiologic differences to explain the difference in drowning risk, race and ethnicity are likely a proxy for social and cultural differences between the groups,” the report adds.
A look back at U.S. history also helps explain why Black children and their parents are less likely to swim. Black families had limited access to public swimming pools not only during segregation but also afterward.
“When public swimming pools were racially desegregated, the reaction to that was for individuals and communities to invest money in private swimming pools,” says Jeff Wiltse, a history professor at the University of Montana and author of the 2010 book “Contested Waters: A Social History of Swimming Pools in America.” “The shift from public provision to private provision was in large part, not entirely, but was in large part driven by racial desegregation.”
Many public swimming pools closed and for Black families who didn’t have the means to join private clubs or pay for expensive swimming lessons, lack of access to public swimming pool continued after desegregation in the 1960s.
“This past discrimination casts a long shadow,” writes Wiltse in his 2014 paper “The Black-White Swimming Disparity in America: A Deadly Legacy of Swimming Pool Discrimination,” published in the Journal of Sports and Social Issues. “As a result of limited access to swimming facilities and swim lessons and the unappealing design of most pools earmarked for Blacks, swimming did not become integral to the recreation and sports culture within African American communities.”
Wiltse says that lack of access to swimming pools is “largely responsible for this contemporary disparity,” and says that generally, lack of swimming ability contributed to drowning deaths.
“In my mind, the lower swimming rates among Black Americans partly contributed to the higher drowning rates,” he says.
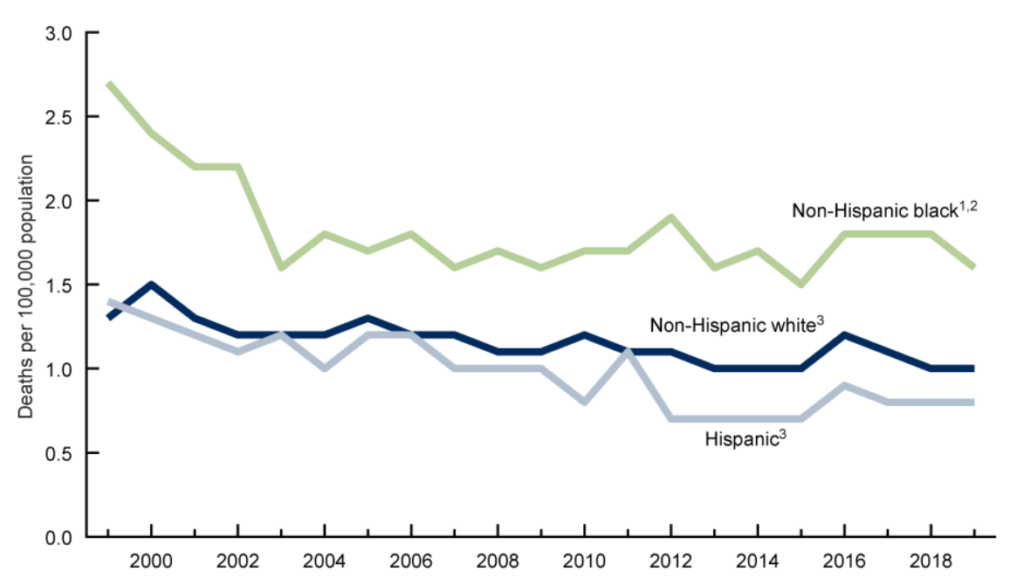
Source: National Center for Health Statistics’ study “Unintentional Drowning Deaths Among Children Aged 0–17 Years: United States, 1999–2019.”
Drowning disparities among American Indian and Native Alaskan youth
There’s a dearth of research on what’s driving drowning disparities between American Indian and Alaska Native youth compared with whites.
“Swimming skill and other factors contributing to increased drowning risk in AI/AN persons have not been thoroughly explored,” write the authors of the June CDC study.
But Dean Seneca, CEO and founder of the consulting firm Seneca Scientific Solutions+ and an adjunct professor at the University at Buffalo who is teaching a class on Indigenous health disparities, points to a few contributing factors.
Many reservation communities don’t have swimming pools, he says.
“Our exposure to swimming at a very early age is very limited if you compare that to other populations,” says Seneca, a Seneca Indian.
In Alaska, even though many of the villages are by the water, people rarely go for a swim because the water is cold, even in the summertime. The majority of the villages don’t have swimming pools, Seneca says.
Also, Alaska Natives are more likely to have water-related jobs, without proper safety equipment, thus increasing their risk of drowning. Many go fishing and practice subsistence to feed their family.
“Did they go on ice with their snowmobile? Was it working properly? Were they putting themselves in a risky situation?” says Seneca, adding that many drownings happen under the influence of alcohol or other substances.
And in many tribes, a focus on swimming is not a top priority.
“We don’t have the prevention messaging in many communities to educate on the seriousness of swimming and drowning,” he says. Also, “look at the Navajo Nation and many of our tribes in the Southwest. They’re struggling just to have water. They don’t even have running water to drink. A pool is probably a last priority.”
Seneca advises journalists to dig deeper into data by looking at Indian Health Services’ reports and contacting tribal epidemiology centers for more information.
Interventions work but they take funding, which Seneca says is severely lacking.
In the widely-cited 2003 study “Reducing Injuries Among Native Americans: Five Cost-Outcome Analysis,” published in Accident Analysis & Prevention, researchers reported that drowning rates dropped by 53% after local residents who used Alaska’s Yukon and Kuskokwim rivers as the primary mode of transportation were offered light-weight coats that doubled as floatation devices.
“To sell the floating properties of the coats to the public, tribal elders suggested a culturally appropriate marketing message: ‘Wear a float coat so that if you drown, people will not have to drag the river for your body,'” the authors write. “This message resonated strongly with communities accustomed to hours and days of uncertainty surrounding most drownings.”
Role of income
Studies haven’t shown that income level is an independent predictor of swimming ability, but some studies have shown an association.
In “Childhood unintentional injury: The impact of family income, education level, occupation status, and other measures of socioeconomic status. A systematic review,” published in Feb. 2021 in Pediatrics and Child Health, researchers looked at 54 studies between 1997 and 2017 on children 19 years and younger. They found that while most studies report higher injury rates among lower-income populations, results vary based on the type of injury and factors such as parental income or education and household size. For instance, 18 of the studies found a significant relationship between income and unintentional childhood injuries. Six studies that focused on traumatic dental injuries found no significant association, while three others did. One study reported that high family income was associated with an increased risk of traumatic dental injury in children.
Of the 54 studies, only one study, from Bangladesh, looked at drownings and found that a mother’s education was a risk factor of increased childhood drowning deaths, the authors report.
In its new report, the American Academy of Pediatrics writes that “inadequate funding for pools, swimming programs, and lifeguards, as well as the cost associated with swimming lessons, may affect water competency and community resources for low-income populations.”
Wiltse calls this a class-based disparity.
“We’re going to find, especially in children of poor and working-class Americans of all races, drowning at a much higher rate than the children of middle- and upper-class Americans,” he says. “I think that’s the piece that the media reporting hasn’t begun to recognize. And unless we reverse, and again reinvest in public swimming pools and swim lessons at public pools, I think we’re going to see worsening of growing drowning disparities along class lines.”
Role of climate change and the COVID-19 pandemic
Some studies are starting to show that warmer winters could result in more fatal drownings.
In the study “Increased winter drownings in ice-covered regions with warmer winters,” published in PLOS One in Nov. 2020, researchers found that winter drownings increased as winter air temperatures got warmer and closer to 32 F, partly because ice covers on bodies of water became more unpredictable.
“The complex nature of changing winters including warming temperatures, rain on snow, and freeze-thaw events could decrease the stability of ice, suggesting that the risk of winter drowning may increase until lakes become completely ice-free,” the authors write.
Researchers used detailed data from Minnesota and found that the most vulnerable age groups for winter drowning were children and young adults. Most children drowned while playing or skating on thin ice. “The risk of drowning was exacerbated by curiosity, inadequate supervision, and a lack of risk-awareness and water-safety education,” the authors write.
As for the COVID-19 pandemic and its impact on drowning death rates in 2020 and so far this year, some local news reports have documented increases. The Boston Globe reported 18 drownings in Massachusetts in May, more than the previous three Mays combined. MLive reported 56 drownings in Lake Michigan in 2020, breaking the previous record of 49 in 2012. And according to the StarTribune, more people have drowned in Minnesota so far this year than in the same period for each of the past nine years.
Meanwhile, home pool sales increased by 21% last year compared with 2019, according to ConsumerAffairs.
But there’s a lag in government data analysis and it might be too soon to tell whether a year of isolation and canceled activities like swimming lessons have led to a significant increase in fatal drownings nationwide.
“We have not been able to look at the data yet,” says Clemens of CDC. “We’re waiting for the final 2020 data to be able to look at whether there’s actually a significant difference in drowning numbers over previous years.”
Solutions
Many studies on drowning call for promoting basic swimming and water safety skills, installing barriers around pools, proper use of life jackets, active supervision of kids in the water and knowing how to perform CPR.
In his aforementioned study, Wiltse writes, “affordable, accessible, and, most importantly, appealing swimming pools are needed to popularize swimming among Black Americans and expand access for poor and working-class Americans more generally.”
A 2023 review of 22 English-language studies on drowning prevention interventions, including research published between 2011 and 2021, finds small but important changes in a range of outcomes. These include changes in awareness, water safety knowledge, attitudes, water safety behaviors and skills, policy changes and drowning rates. The interventions included swimming lessons, mandatory personal floatation devices, awareness campaigns and barriers to prevent access to water. One experimental study, published in 2019 in the journal Injury Epidemiology, finds that posting a sign at a park, informing visitors that water entry was illegal and could result in a fine exceeding $200, reduced the odds of someone entering the water by 63%.
A 2024 review of 47 English-language studies on life jackets finds that overall, life jacket usage is low — but that life jackets are highly effective at preventing drowning when people wear them. The authors underscore the significance of targeted interventions, regulation and educational programs that promote the use of life jackets to reduce drowning incidents. They also highlight the role of health care professionals in educating patients about the benefits and proper use of life jackets.
In the Dec. 2020 study “Adolescent Water Safety Behaviors, Skills, Training and Their Association with Risk-Taking Behaviors and Risk and Protective Factors,” published in Children, Quan and colleagues recommend diversity in swimming education. “Water safety education programs must include input from culturally diverse and immigrant populations throughout program development and implementation and provide information for parents in languages other than English,” Quan and colleagues write. “Furthermore, it’s essential that water safety programs recruit and retain lifeguards, swimming instructors, program administrators, and educators that reflect the communities that they aim to reach.”
Some researchers also suggest including water safety training in school curriculums.
Shawn Slevin, executive director of Swim Strong Foundation, a nonprofit organization in New York City, is working on legislation to mandate water safety training in New York State schools.
The Pew Charitable Trusts’ Stateline reported on July 15 that drowning prevention could be getting a boost in the federal budget. The story also provides a roundup of drowning prevention legislation in several states.
“The ability to enter a safe body of water during a warm summer is one of the real pleasures of life,” says Wiltse. “It’s an escape from the heat. It’s refreshing. It’s rejuvenating. It’s physically pleasurable. It’s mentally healthy and physically healthy. And I think it’s a matter of social justice. All people should have access to safe swimming venues. And just because you’re poor, working class, you shouldn’t be deprived of that pleasure.”
Story ideas and sources of drowning data
Check your community for local organizations that are offering free or no-cost swimming lessons to children and adults.
Check your county or state health department website for local and state data. Also check Indian Health Services’ reports and contact tribal epidemiology centers for more local information.
CDC’s WISQARS [Web-Based Injury Statistics Query and Reporting System] provides an interactive database about fatal and nonfatal injuries, violent deaths and cost of injury data.
CDC WONDER [Wide-ranging ONline Data for Epidemiologic Research] is another source of data. Use this Quick Start guide to learn how to use the system.
CDC’s Drowning Prevention website provides state-by-state drowning death rates.
Water Safety USA is a roundtable of several national nonprofit and governmental organizations with a focus on drowning prevention and water safety programs. The group is planning to publish the first-ever U.S. National Water Safety Action Plan, Pew’s Stateline reports.
The American Red Cross is another good source of drowning prevention information and facts.
If you’re looking to put together an info box for drowning prevention measures, the American Academy of Pediatrics and the CDC have helpful bullet points.
If you’re looking to learn more about disparities in recreational activities, here are three books to get you started: “Race, Riots, and Roller Coasters: The Struggle Over Segregated Recreation in America” by Victoria Wolcott. “The land was ours: how black beaches became white wealth in the coastal south” by Andrew Kahrl. “Contested Waters: A Social History of Swimming Pools in America” by Jeff Wiltse.
Remember that The Journalist’s Resource publishes its content under a Creative Commons license, meaning you’re free to republish this piece in your own news publication, provided you include author credit and a link back to the original piece. You’re also welcome and encouraged to embed the map and the Swimming Safety Tips graphic into your own stories.


Expert Commentary