The United States spends 17.9% of its gross domestic product (GDP) on health care, the most of any country in the world. In contrast, Canada’s health spending makes up 10.9% of its GDP and the United Kingdom spends 9.4%. Despite a significantly higher level of expenditures, U.S. residents experience poorer health by most metrics in relation to their counterparts in Canada, Britain and other high-income nations: U.S. lifespans are shorter, infant mortality rates are higher, obesity is more common and mental health is generally poorer. Prolonged exposure to life in the United States also seems to make people sicker. When immigrants first come to the United States their health is usually better than that of the average American, but — over time — they come to resemble their U.S.-born counterparts, with increased rates of heart disease, hypertension, diabetes and other ailments.
High levels of health care spending cannot guarantee a healthier populace; there are many other factors that influence the rates of disease, injury and death that a society experiences. These factors are known as “social determinants of health,” defined by the World Health Organization as “the conditions in which people are born, grow, live, work and age [that are] shaped by the distribution of money, power and resources at global, national and local levels.” Policies regulating air pollution, national income distributions and racially discriminatory laws, or the presence or absence of bicycle paths and green space in neighborhoods are just some examples of the social determinants of health.
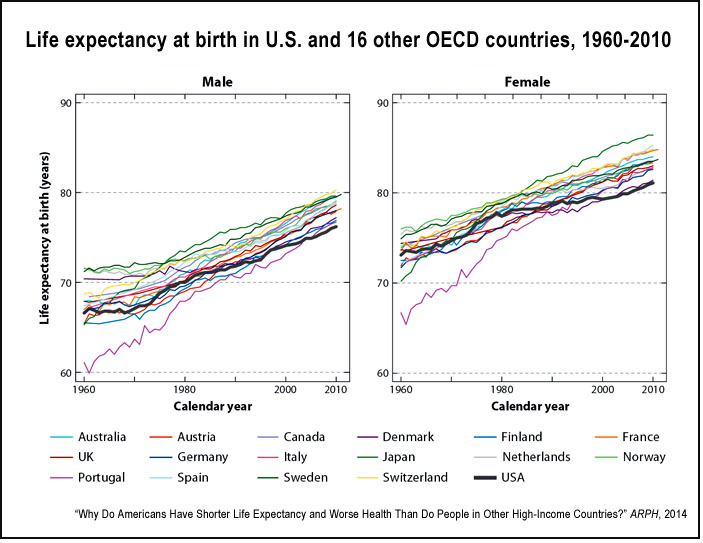
A 2014 review article in the Annual Review of Public Health, “Why Do Americans Have Shorter Life Expectancy and Worse Health Than Do People in Other High-Income Countries?” assesses various explanations for the U.S. health disadvantage with a focus on life expectancy. The authors — Mauricio Avendano of the London School of Economics and Ichiro Kawachi of Harvard University — compare mortality in the United States with that in 16 other high-income countries (Australia, Japan, Canada and 13 Western European nations).
A summary of the article’s findings includes:
- The United States has the lowest life expectancy at birth for both women (80.6 years) and men (75.6 years) compared to the other 16 nations. According to a 2013 study from the University of Pennsylvania, higher mortality rates before age of 50 accounts for much of the difference. Among the countries studied, men lived longest in Switzerland (79.8 years) and women lived longest in Japan (86.1 years).
- There are wide disparities in U.S. life expectancy by geography, race and socioeconomic status. A 2006 analysis in PLoS Medicine found that black men living in urban areas are expected to die 21 years earlier compared to the national average for Asian women. Life expectancy also varies by U.S. region — people in the South and Midwest are expected to live the shortest lives, while those in New England and on the West Coast live the longest. These inequalities may explain some of the U.S. health disadvantage relative to other countries. The authors note that among low-income Americans, rates of homicide and HIV/AIDS-related deaths are very high. However, a 2009 study found that even white, middle-class Americans (a relatively healthy demographic group by U.S. standards) experience poorer health than their European counterparts.
- Differences in health insurance and the health care system may explain part, but not all, of the U.S. disadvantage in mortality. While lack of universal health care coverage may be detrimental to health, even Americans with insurance have poorer health than Europeans. Additionally, there is no evidence that American medical care is of poorer quality, and survival rates following certain chronic diseases are in fact higher in the United States.
- Smoking explains only a relatively small part of shorter U.S. lifespans. Because there is typically a decades-long lag between when people smoke and when they fall ill, the United States is still experiencing a high number of smoking-attributable deaths. However, these deaths typically occur after age 50, while most of the relative increase in U.S. mortality occurs before age 50.
- Based on a number of analyses by the National Research Council and others, obesity — a condition on the rise throughout much of the world — does not significantly account for cross-national differences in life expectancy.
- Differences in physical infrastructure may contribute to the differences in life expectancies, but research is lacking. In particular, U.S. communities tend to be car-centric, which limits opportunities for physical activity. Also, people in the United States drive longer distances and, as a result, they are more likely to die in automobile accidents compared to people in other wealthy nations.
The authors conclude that none of the standard explanations sufficiently account for relatively short U.S. life expectancies, but speculate that differences in social policy may play a role: “Ample evidence indicates that social policies and programs affecting Americans across the entire life course are less comprehensive in the United States than in other OECD [Organization for Economic Cooperation and Development] countries.” In particular, a higher level of income inequality in the United States, weaker labor laws and less investment in programs that address housing, poverty, education and childcare may be responsible for the disparity in lifespans. When looking at combined investments in health care and these other social programs, the United States is not the world’s top spender. In addition, the U.S. private sector accounts for a disproportionate share of health and social spending.
“Although the impact of many of these policies on social outcomes is well documented,” the authors write, “the extent to which they influence health and contribute to differences in longevity among high-income countries is yet to be established. Disentangling the role of public policies is crucial to unravel why the most prosperous economy in the second half of the twentieth century continues to lag behind other high-income countries in life expectancy.”
Keywords: poverty, obesity, nutrition, exercise, cars, automobiles, driving

Expert Commentary